Spine endoscopic surgery, which minimizes incisions and reduces infection risk to lessen the burden on patients, is gaining attention from spine specialists worldwide. At the center of this field, which Korea leads, is Professor Jin-Sung Kim, who transfers surgical techniques to Global medical professionals and drives improvements in global healthcare quality.

The value of medical technology, which ultimately aims to alleviate patient suffering and improve quality of life, grows even greater when it spreads across borders. While the number of patients a single doctor can treat is limited, sharing technology allows more patients to receive standardized treatment regardless of location. Meanwhile, the international spread of cutting-edge technology also means accelerating medical advancement. Feedback from diverse clinical environments creates a virtuous cycle leading to the development of the technology itself and establishes a platform for knowledge exchange among experts to improve global healthcare quality.
A prime example is minimally invasive spine endoscopic surgery. Single-port endoscopic surgery has more than 30 years of history but has developed very slowly due to the long time required to master surgical techniques and the high cost of endoscopic instruments. However, since the introduction of bi-directional spine endoscopic surgery at the World Federation of Neurosurgical Societies in 2013, it has achieved remarkable development through continuous technological innovation by Korean Spine suregeons. The single-port transforaminal endoscopic surgical method can be performed under local anesthesia and is useful for disc herniation but has limited application for spinal stenosis, which is common in elderly patients. In contrast, the bi-directional endoscopic surgical method is an effective treatment for spinal stenosis common in elderly patients through epidural or general anesthesia. As Korea emerges as a leading country in the development and advancement of new spine surgical techniques, spine specialists from the United States, Europe, and other countries are visiting Korea to learn these surgical methods.
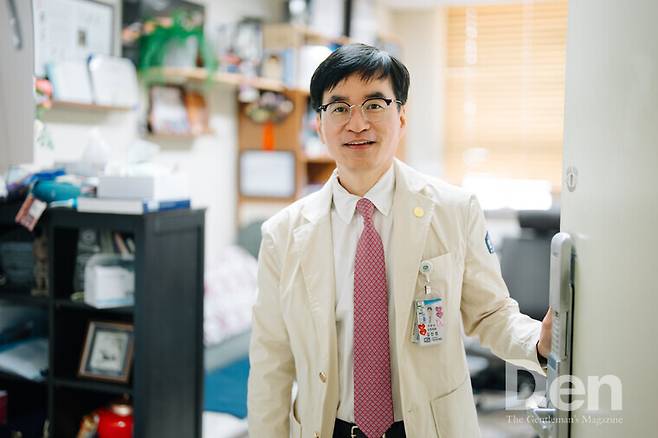
Professor Jin-Sung Kim, a neurosurgery specialist at Seoul St. Mary's Hospital, is a world authority on minimally invasive spine endoscopic surgery. Having accumulated various papers and clinical experiences in the fields of spine endoscopic surgery and minimally invasive spine fusion surgery, he authors textbooks and conducts lectures on spine endoscopic surgery for spine specialists worldwide to transfer his techniques. Dedicated to research and education while contemplating better treatment methods, he is both a mentor in the field of spine endoscopic surgery and a reliable companion to numerous patients with spinal disorders.

He graduated from the Catholic University of Korea College of Medicine in 1997 and obtained his master's and doctoral degrees in neurosurgery from the same graduate school. After six years of clinical experience at Wooridul Hospital, he has been serving as a professor of neurosurgery at Seoul St. Mary's Hospital since 2012. He has authored over 200 papers and textbooks published by global publishers on spine endoscopic surgery. He serves as an expert committee member of ISO in spine surgery standardization, International Chair of the Society for Minimally Invasive Spine Surgery (SMISS), and Deputy Editor of international spine journals "Global Spine Journal" and "Neurospine." Currently, he performs minimal invasive spine and spreads especially endoscopy surgical techniques to spine surgeons worldwide through lectures.
Many modern people complain of spinal disorders. Is the annual number of spine surgeries also increasing?
Spine surgery is performed so frequently that it ranks within the top three in the frequent surgery statistics published by the National Health Insurance Service every year. Indeed, the number of surgeries has been steadily increasing. In 2021, about 128,000 procedures were performed, but by 2024, this number has exceeded 155,000. This figure only accounts for data claimed to the Health Insurance Review and Assessment Service, so if we include surgeries performed as non-covered items in private hospitals, the actual proportion of surgical and non-surgical treatments for spinal disorders would be much higher.
As the demand for spine surgery increases, attention is focused on minimally invasive spine endoscopic surgery as the latest method. What is spine endoscopic surgery?
Instead of incising both skin and muscle, it is a surgical method that treats spinal disorders by making a skin incision of about 1cm and inserting an endoscope. The method of incising the skin on only one side and proceeding with surgery is called unilateral endoscopic surgery, while the method of incising both sides and inserting an endoscope and surgical instruments is called Biportal endoscopic surgery. Currently, disc herniation and stenosis can be treated with endoscopic surgery. About 15 years ago, it was only applied to disc herniation, but since 2014, as technology has advanced, stenosis can also be treated endoscopically. Currently, I use endoscopy or minimally invasive fusion techniques in about 90% of the surgeries I perform.
What are the absolute indications that require surgical treatment?
Stenosis is difficult to recover naturally, so surgery is necessary to alleviate symptoms once it reaches a critical point. Disc herniation, the most common spinal disorder, can lead to cauda equina syndrome with urinary, bowel, and sexual dysfunction if nerves within the spinal canal are damaged. Without appropriate surgical treatment, there is a high possibility of permanent nerve damage, so surgery is recommended. Surgery is also necessary in cases of progressing paralysis, such as foot drop paralysis. However, since disc herniation can recover naturally, if the disc has slightly protruded causing leg numbness, it is common to monitor the progress for two to three months while receiving non-surgical treatment before deciding on surgery.
What are the advantages of spine endoscopic surgery?
What spine specialists fear most is infection. During my residency, I saw many patients who had long-term hospitalizations due to inflammation after spine surgery. Open surgery has relatively larger invasive areas, and there is a possibility of partial muscle damage during the process of pulling with a retractor after skin incision. This makes it easier for bacteria introduced from outside to adhere and cause inflammation. Usually, when such inflammation occurs, antibiotics must be administered for at least 6 weeks, or even more than 3 months in some cases. In contrast, spine endoscopic surgery, which does not require extensive skin and muscle incisions, has an infection probability approaching 0%. The minimal risk of infection can be considered its greatest strength.
Can elderly patients also undergo surgery?
For the elderly, general anesthesia increases the possibility of cardiopulmonary dysfunction or internal medical complications. Spine endoscopic surgery can be performed under partial anesthesia and has a lower risk of infection, making it less burdensome. In fact, I recently performed endoscopic surgery on a 92-year-old stenosis patient. After disc surgery 10 years ago, that patient had developed stenosis and instability in the area, requiring surgery to insert artificial bone and fixation, but was hesitant due to concerns about general anesthesia. So, I injected only local anesthetic into the surgical site, removed the overgrown bone and disc endoscopically, inserted artificial bone, and fixed it with screws. The patient is now doing well without pain. This may be the first case in Korea where endoscopic fusion surgery was performed under local anesthesia for such an elderly patient.
Are there any disadvantages to endoscopic surgery?
When skin is incised, bleeding inevitably occurs. Patients taking aspirin-type medications due to underlying diseases or those with low platelet counts may bleed more than others. Although endoscopic surgery results in less bleeding than open surgery, controlling bleeding can be somewhat difficult. This is because the use of instruments is limited, and even small bleeding can cause the field of view to become cloudy. However, cases where surgery cannot be performed due to hemostasis issues are rare. Although hemostasis may take longer than in open surgery, most procedures proceed smoothly.
I wonder why you are dedicated to research in this field.
A doctor should always be able to suggest appropriate surgical methods that meet the patient's needs. For young patients, there may not be much difference in results whether performing microscopic surgery with a somewhat larger incision or endoscopic surgery. However, for patients with underlying diseases or elderly patients, endoscopic surgery is much more advantageous in terms of recovery speed and risk of complications. The broadening spectrum of diseases that can be treated with endoscopic surgery means that patient-centered treatment is possible. Especially since our country is an aging society, I thought it necessary to research surgical methods that benefit elderly patients.
There must have been many trials and errors in the early days of technology adoption.
"First movers" who quickly adopt and start new technologies inevitably learn through trial and error. Spine endoscopic surgery is no exception. Especially endoscopic surgery has a very steep learning curve. When I started endoscopic surgery, there weren't many people who could teach the techniques, so in the early stages of adoption, results were not perfect, and complications sometimes occurred.
To achieve good surgical results by applying the latest surgical methods, it is essential to share results with domestic and foreign medical professionals and report success and failure cases through papers. I also reviewed other medical professionals' surgical results and actively shared detailed reports when complications occurred. Because of these trials and errors, I advise my disciples to carefully examine unfavorable surgical results. Learning from failures ultimately leads to technological advancement.
You've treated numerous patients so far. Are there any memorable cases?
Although not quite a genetic disease, spinal disorders often have a strong family history. Just as parents and children resemble each other's faces, spine shapes also tend to be similar. Recently, I performed surgery on a man in his early 40s. About 5 years ago, his father had surgery with me, and 9 years ago, his grandmother also received surgery from me. Because spinal disorders tend to run in families, it's not uncommon for two generations—such as a father and son or a mother and daughter—to undergo surgery. However, this was my first time operating on three generations, which made it especially memorable.
You not only perform surgeries but also transfer know-how to Global medical professionals. In which countries have you given lectures so far?
Before the COVID-19 pandemic, there were many lecture requests from China, so I gave more than twelve lectures in China and one or two in the United States annually. I also visited numerous other Asian countries, and to fulfill my overseas schedules, I used all my personal vacations except for two official leaves granted by the hospital. So, for 13 years, I've never used personal vacation time for my family. Instead, I attend conferences with my family once a year. Since the end of the pandemic, as Korean endoscopic surgery has influenced the world, I mainly visit the United States, Latin America, Europe, and the Middle East. Looking at my international conference activity statistics for 2024, I participated in 75 academic activities, including 51 invited lectures, 6 chairmanships, and 17 cadaver training sessions in countries such as the United States, Brazil, Colombia, Switzerland, Saudi Arabia, Spain, Hong Kong, and Thailand.
How many trainees have you had so far?
I've guided about 40-50 trainees so far. Because I want to nurture foreign trainees into true leaders in the field of spine endoscopic surgery, I don't accept short-term training of less than 6 months and usually train only about 4 trainees at a time. Among the trainees who have completed the fellowship program, some disciples have become world authorities who are invited to give lectures. I feel a great sense of fulfillment when I see that.
Is there a reason you started activities targeting global medical professionals?
Even just 20 years ago, discussions about minimally invasive surgeries like endoscopic surgery were not actively held at domestic conferences. At that time, most professors mainly performed open surgeries through incisions, so the concept of operating through a small hole of about 1cm might have seemed unrealistic to them. The atmosphere wasn't as open as it is now for new attempts like minimally invasive fusion surgery and minimally invasive lateral surgery. So, for about 5 years from 2008, I mainly engaged in international conference activities centered on the United States and conducted paper and research activities. The international conference activities that started then have continued until now.

I'm curious about the current level of spine endoscopic surgery in Korea.
Just as K-pop and K-culture are famous, there is also 'K-Spine Power' in the field of spine endoscopic surgery. The surgical skills of doctors, as well as the quality and influence of related academic papers, are excellent, attracting significantly more foreign trainees than other surgical fields. Just 5 years ago, there were few experts who could teach spine endoscopic surgery in Europe, and even in the United States, only limited surgical techniques were available. However, now doctors trained in Korea are returning to their countries, organizing conferences, and inviting their Korean mentors to hold sizeable conferences in Europe, South America, and other regions. These changes are good examples that demonstrate the status and level of Korean spine endoscopic surgery.
Besides training fellows, you also interact with global medical professionals through international journals and conference activities.
Currently, I serve as Deputy Editor of "Global Spine Journal" and "Neurospine," and as an editorial board member of "Eurospine." Particularly at "Neurospine," the Korean Society of Spine Surgery's journal ranked 2nd in impact factor among spine journals, I review submitted research papers and participate in making final publication decisions. Also, since 2018, I have been the only Asian executive of the AO Spine Minimally Invasive Spine Surgery Committee, and since last year, I was elected as a director of the North American Spine Society (NASS) International Strategy and Growth Committee (ISGC), working on international networking for NASS's influence expansion. When NASS holds joint conferences in other countries, I create and teach endoscopic surgery courses as a representative and communicate with specialists at international conference venues.
Among your various experiences on the international stage, was there a turning point in your medical career?
I attended the Global Spine Congress (GSC) in 2017. Created by the AO Spine global academic community, the GSC is considered one of the world's largest spine conferences along with NASS and EuroSpine. At that time, I was asked by the GSC chairman to create educational content for minimally invasive surgical methods like endoscopy, so in 2018, along with other Korean colleagues, we established a spine endoscopic surgery training course at the Singapore GSC, which continues to this day. Subsequently, I created and chaired the first spine endoscopic surgery education course at the "Davos Course," the highest educational event conducted by AO Spine.
These opportunities allowed me to actively create presentation opportunities for Korean medical professionals in endoscopic surgery-related sessions at major spine conferences worldwide and serve as a bridge for official cooperation between Korean and international conferences. I acted as a kind of ambassador. In recognition of these contributions, I received the International Service Award from the Korean Society of Minimally Invasive Spine Surgery. I consider these experiences meaningful beyond personal achievement, as they have helped make Korea's spine surgery technology known to the world and raised its international status.

What research area are you currently focusing on?
While the United States has officially assigned codes for disc herniation, stenosis, foraminal surgery, and cervical/thoracic endoscopic surgery since 2017, in Korea, spine endoscopic surgical methods have not yet entered the institutional framework of the Health Insurance Review and Assessment Service. As a researcher in this field, this reality is truly regrettable. Therefore, with the goal of definitively incorporating endoscopic surgical methods into the institutional framework before retiring from active practice, since 2021, I have been conducting a large-scale government project called "Patient-Centered Medical Technology Optimization Research Project" together with experts from major domestic medical institutions such as Seoul National University Bundang Hospital, Daejeon St. Mary's Hospital, Hallym University Hospital, Chung-Ang University Hospital, Severance Hospital, Cheongdam Wooridul Hospital, and Wills Memorial Hospital. I am also conducting a government project called "Wide Area Korean Medical Device Education and Training Support Center Support Project" to discover and support related domestic companies.
To introduce a new surgical method into Korea's institutional framework, robust clinical evidence must be prepared. By performing research tasks on government-designated focus diseases, academic evidence and data are accumulated, and once the results are proven, incorporation into the institutional framework becomes possible. Currently, we are collecting data to prove the efficacy and safety of spine endoscopic surgery by comparing traditional surgical methods with endoscopic surgical methods for patients with stenosis and disc herniation. At present, patient recruitment has been completed, and we are at the stage of examining and observing patients. I expect that outstanding research results will be published within the next 3-4 years, providing evidence for spine endoscopic surgery to enter the institutional framework.
What drives you to combine clinical practice and research?
I find fulfillment in discovering new things and taking on new challenges. Research holds as much importance to me as clinical practice and surgery. I believe the core driving force is the fulfillment gained when my colleagues and I experience moments where our academic contributions reduce patient pain, aid rapid recovery, and change the indications in textbooks. Moving forward, I want to broaden the range of diseases that can be treated with new surgical methods to bring more benefits to patients.
I'm curious about your ultimate goal as a doctor.
The term 'ultimate goal' seems unsuitable for clinicians. If you asked a soldier fighting on the battlefield every day about their wish, they would probably answer, "being given tomorrow." Rather than any goal, I want to walk the path of a "命醫" (physician with a mission) rather than a "名醫" (famous physician). I want to live as a doctor who has received the command to "care for patients and conduct research" rather than as a famous and accomplished doctor.
ㅣ 덴 매거진 2025년 5월호
에디터 김보미 (jany6993@mcircle.biz)
사진 송승훈 포토그래퍼
Copyright © 저작권자 © 덴 매거진 무단전재 및 재배포 금지